Share
Bedsores, also known as pressure ulcers or decubitus ulcers, are serious skin injuries that form from prolonged pressure on the skin. These wounds can range from mild discomfort to severe pain if left untreated, which is why it’s critically important to focus on bed sore prevention for clients who are limited to bed rest.
This guide will explore what causes bed sores, the different stages, and effective prevention strategies for clients.
What Causes Bed Sores?

Photo 28705824 © Monkey Business Images | Dreamstime.com
Bed sores develop when pressure on the skin restricts blood flow, leading to tissue damage. They commonly occur where bone lies close to the skin, like the heels, ankles, hips, and tailbone.
People with medical conditions that limit their ability to change positions, or those who spend long periods in their bed or chair, are at the highest risk of developing bed sores.
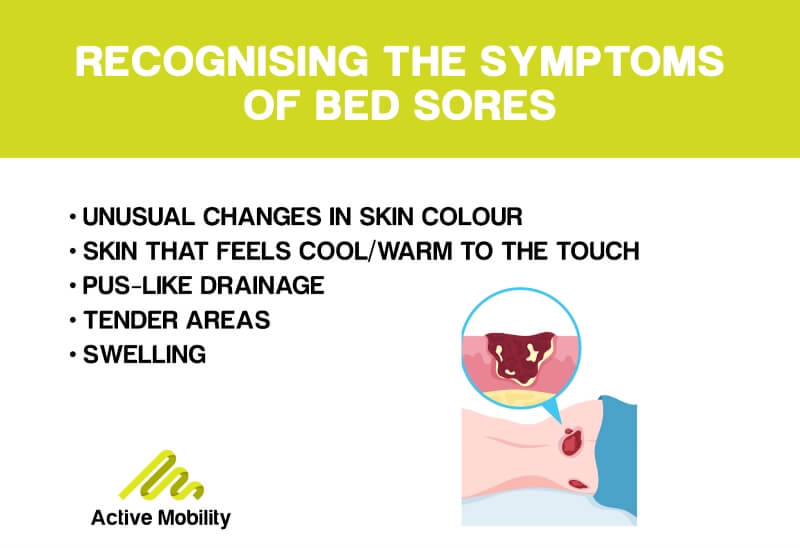
Recognising The Symptoms
Spotting the warning signs of bed sores is crucial for early intervention and treatment.
Bed sores are categorised into different stages, each representing varying degrees of skin and tissue damage. The stages range from changes in skin colour to deep injuries involving muscle and bone.
The location of bed sores differs depending on whether the person is using a wheelchair or confined to a bed. For wheelchair users, pressure ulcers often form on the tailbone or buttocks, shoulder blades and spine, and backs of arms and legs where they rest against the chair.
For individuals who need to stay in bed, bed sores may develop on the back or sides of the head, shoulder blades, hip, lower back or tailbone, heels, ankles, and skin behind the knees.
Stages Of Bed Sores
Understanding the stages of bed sores is essential for effective treatment and management. This staging system can help determine the severity of a bed sore:
- Early Signs: In the initial stage, the skin may appear red or pink and feel tender to the touch. It may also feel warmer, cooler, softer, or firmer than the surrounding areas.
- Shallow Wound: A shallow wound with a pink or red base may develop at this stage. Skin loss, abrasions, and blisters may also be present.
- Deeper Wound: A noticeable wound that extends into the skin's fatty layer (hypodermis) is characteristic of stage 3 bed sores. The affected area may exhibit a crater-like appearance.
- Severe Damage: Here, the wound penetrates all three layers of skin, exposing muscles, tendons, and bones. The depth of the wound may vary, and the surrounding tissue may appear necrotic or dead.
Complications & Risks
Bed sores can lead to various complications, some of which can be life-threatening. These complications include:
- Cellulitis: An infection of the skin and underlying soft tissues, causing inflammation, warmth, and swelling.
- Bone and Joint Infections: Infections from pressure sores can spread to the bones and joints, leading to joint damage or reduced limb function.
- Cancerous Development: Long-term, non-healing wounds can develop into squamous cell carcinoma known as Marjolin's ulcers.
- Sepsis: In rare cases, a skin ulcer can lead to sepsis, a severe infection that can spread throughout the body.
How To Prevent Bed Sores

Photo 35803267 © Monkey Business Images | Dreamstime.com
Prevention is key when it comes to bed sores. Taking proactive measures can reduce the risk of developing these painful wounds. Here are some effective strategies for prevention.

RepositioningFor bed-bound clients, change positions at least every two hours. Use pillows or foam wedges to keep knees or ankles from touching and elevate heels off the bed. For wheelchair users, shift weight approximately every 15 minutes. This can be done by leaning side to side, forward, or using a tilt-in-space wheelchair if possible. |
Support SurfacesUse specialised mattresses and cushions made from foam, air, or gel that redistributes pressure. |
Regular ChecksLook for early signs of pressure sores, including redness, warmth, swelling, hardness, or pain in the area. Pay special attention to bony areas such as the tailbone, hips, heels, and elbows. |
SkincareMaintaining good skin hygiene is essential to prevent bed sores. Keep the skin clean and dry, use gentle cleansers and avoid scented soaps. Moisturise the skin thoroughly after washing and use moisture barrier creams to protect against moisture from sweat, urine, or stool. |
Nutrition & HydrationEnsure the client’s diet is high in protein, vitamins (especially A and C), and minerals. Consider supplements if needed. Aim for adequate fluid intake unless medically contraindicated. |
Shear & FrictionUse lifting devices like grab bars for bed-bound clients. For wheelchair users, use soft, non-binding clothing and smooth sheets to reduce friction. |
Personalised Care PlansDevelop a tailored care plan considering the individual's health needs and risks, and have health professionals evaluate the individual’s skin condition regularly. |
ExerciseEven minimal movements can improve circulation. These can be assisted or passive exercises if the person cannot move independently. Always consult a physical therapist for appropriate exercises. |
RepositioningFor bed-bound clients, change positions at least every two hours. Use pillows or foam wedges to keep knees or ankles from touching and elevate heels off the bed. For wheelchair users, shift weight approximately every 15 minutes. This can be done by leaning side to side, forward, or using a tilt-in-space wheelchair if possible. |
Support SurfacesUse specialised mattresses and cushions made from foam, air, or gel that redistributes pressure. |
Regular ChecksLook for early signs of pressure sores, including redness, warmth, swelling, hardness, or pain in the area. Pay special attention to bony areas such as the tailbone, hips, heels, and elbows. |
SkincareMaintaining good skin hygiene is essential to prevent bed sores. Keep the skin clean and dry, use gentle cleansers and avoid scented soaps. Moisturise the skin thoroughly after washing and use moisture barrier creams to protect against moisture from sweat, urine, or stool. |
Nutrition & HydrationEnsure the client’s diet is high in protein, vitamins (especially A and C), and minerals. Consider supplements if needed. Aim for adequate fluid intake unless medically contraindicated. |
Shear & FrictionUse lifting devices like grab bars for bed-bound clients. For wheelchair users, use soft, non-binding clothing and smooth sheets to reduce friction. |
Personalised Care PlansDevelop a tailored care plan considering the individual's health needs and risks, and have health professionals evaluate the individual’s skin condition regularly. |
ExerciseEven minimal movements can improve circulation. These can be assisted or passive exercises if the person cannot move independently. Always consult a physical therapist for appropriate exercises. |
Find Bed Sore Prevention Products Online At Active Mobility
The risk of pressure sores can be significantly minimised if you commit to the prevention techniques listed above. Both individuals at risk and support workers need to be proactive in preventing these sores — they can be difficult to treat once they develop.
At Active Mobility, we provide holistic care for our customers and stock bed sore prevention products like specialised mattresses, cushions, and even skincare products. Shop the range online for fast, affordable shipping, or contact us for personalised recommendations and advice from our occupational therapists.